Job Market Re: Australia
Hi :) I'm considering doing optom at unsw next year and I was wondering how the job prospects are currently? I've heard that it'll be a saturated job market in the next few years so I'm not if its a worthwhile investment, as I'm from WA and although I'm genuinely interested, a really big factor is the $ ahaha. Also I was wondering what the community life at the uni, since I'm a bit worried I wont make any friends lmaoo? Also how difficult is the workload as compared to year 12? Thanks so much <3
Job Market re: Australia
Hey! Keep in mind, this is what info I’ve been hearing from colleagues as well as some optometrists who are hiring. If you’re from WA, then I would say that you don’t have to worry about saturated job markets if you’re going to return to your home state after graduating. I’ve heard you can get $100K starting salary even relatively close to the city. Melbourne and Sydney though are probably closer to hitting saturation, but they’re capping university take ins next year, so again it could be a completely different ballgame by the time you get out in Sydney and Melbourne. WA though is totally safe, I believe they’re underserviced because there are no optometry schools there. And of course, anywhere that is regional or rural, regardless of state is underserviced, so if you’re cool with moving out to learn a bit more about using your therapeutic skills and ocular disease, then there should be absolutely no problem. Job prospects are only a bit riskier staying with Syd/Melb metro.
Student Life re: UNSW
Pretty friendly on the whole, I believe that because UNSW is one of the newer universities, even the aura here is a bit more cosmopolitan. We definitely have many international students, and also there are a lot of 1st years who are super bubbly because 1) it’s a new experience and they’re excited and 2) it’s a new environment and they’re apprehensive about making friends. So literally everyone feels the same way and as long as you make a little effort to get to know someone, it’ll be more than reciprocated. Just large cliques of high school friends may be trickier to break, because it’s difficult to broach friendship with someone who’s already 6 years deep in friendship with others and still not interested in making new friends.
Also, see these posts that I’ve written about making friends because I keep getting questions about it somehow LOL
Making Conversation - a guide for introverts!
Making Friends
Part 4 Extra-Curriculars
Part 6 Social Life
High School vs. University Workload
As a precursor, no matter what the degree, studying anything at a tertiary level is going to be a challenge, not necessarily difficult. Particular degrees might be easy/hard to particular people, etc. If you’d like to know more about university I have a whole series on it.
Read this for a summary: Transitioning from High School to University
Part 0 Choosing a Degree
Part 1 Administration
Part 2 Getting to Class - pros and cons of attending class, when you should choose not to attend, laptop and notebook recommendations, advice about choosing a backpack and other essential equipment.
> Laptop Considerations and Recommendations
Part 3 Studying
Part 4 Extra-Curriculars
Part 5 Exams
Part 6 Social Life
Part 7 Part Time Work
Part 8 Four Secrets The Uni Tells You
Part 9 Best Study Spots On Campus
Part 10 Saving Money 1 - Food, Transport, Entertainment
Part 10 Saving Money 2 - Textbooks, Tax, Scholarships
Part 11 Adapting to Uni Study popular!!
Part 12 How to Study From Textbooks in Uni
Part 13 Dealing with Lazy Group Members
But granted, I’m going to say that optometry is hard. Personally I would say, and I’ve also had someone describe to me, that it’s like doing 2 HSC exams every year because of the amount of info that you have to cram into 13 weeks of a semester. I’ve had a guest lecturer who was an ophthalmologist who originally graduated as an optometrist, worked for a while and then did the GAMSAT and post-grad medicine and he told us that optometry was more difficult than the generalist medical degree. I’ve also heard from numerous other people in the field, relatives, and also heard about families with children studying both optometry and medicine saying that optom undergrad is more difficult. This is most likely because the 5 year degree is meant to give you complete training, compared with medicine where you have a 6-7 year undergrad followed by the 3 year hospital training before another 5 years of specialisation.
Be prepared for hard work and long hours. I said this in a previous ask but at the end of the day, the job that you do as an optometrist requires you to keep an eye out for sight-threatening and life-threatening conditions, as well as to deal with common eye problems day to day, so you need to learn a lot about anatomy and physiology, anatomy of the eye/head/brain and the innervation/blood supply, as well as the diseases that can arise, and how to manage and treat them. Refraction and getting an actual prescription is a skill that needs a lot of practice and refinement too.
See these asks for more details about optometry:
Optometry Prerequisites and Difficulty (yes someone’s asked before :)
Why I Chose Optometry and Comparisons to Other Health Sciences
Entry Requirements at UNSW
Format of the Degree and 1st Year Contact Hours
+ general tag for all optometry related asks
Hope that helps! ^_^
More Posts from T-b-a-blr-blog and Others
Innate Immunity - intro
First line of defence + first to act
A primitive response (exists in animals and some plants)
Non-specialised and without ‘memory’
Consists of:
Physical barriers (eg skin and mucosa//tight junctions, airflow)
Chemical barriers (eg enzymes, lung surfactant, antimicrobals)
Soluble mediators of inflammation (eg cytokines)
Microbal defence (eg commensal competition, secreted antimicrobals)
Cells (eg phagocytes)
Receptors to recognise presence of pathogen/injury - results in inflammation

Soluble Mediators
Complement Proteins
liver-derived
circulate in serum in inactive form
activated by pathogens during innate response
functions include lysis, chemotaxis and opsonisation

Auxiliary Cells
Mediate inflammation as part of the immune response. The main auxiliary cells involved in the immune response are Basophils, Mast cells and Platelets.
Basophils
Leukocyte containing granules
on degranulation release histamine + platelet activating factor
causing increased vascular permeability and smooth muscle contraction
also synthesise and secrete other mediators that control the development of immune system reactions
Mast Cells
Also contain granules
However they are not circulating cells - found close to blood vessels in all types of tissue especially mucosal and epithelial tissues.
rapidly release inflammatory histamine but this is IgE dependant so not innate
Platelets
normally function in blood clotting
also release inflammatory mediators

Cytokines and chemokines
Produced by many cells but especially mØ (macrophages), initiate inflammatory response and act on blood vessels
interferons - antiviral protection
chemokines - recruit cells
interleukines - fever inducing, IL-6 induces acute phase proteins
IL-1 - encourages leukocytes to migrate to infected/damaged tissue
as does tumour necrosis factor (TNFa)
Acute phase proteins
Liver derived proteins
plasma concentrations increase (positive acute-phase proteins) or decrease (negative acute-phase proteins) in response to inflammation
called the acute-phase reaction
triggered by inflammatory cytokines ( IL-1, IL-6, TNFα)
help mediate inflammation ( fever, leukocytosis, increased cortisol, decreased thyroxine, decreased serum iron, etc)
activate complement opsonisation
Inflammation

Cells
Cytotoxic Cells
Eosinophils/natural killer cells, cytotoxic T cells
kill target via release of toxic granules
dendritic cell derived IL-12 helps activate NK cells
Phagocytes
mono-nuclear = long-lived; polynuclear = short-lived
engulf, internalize and destroy
phagosome forms around microbe
enzyme filled with lysosomes fuses to form phagolysosome
organism is digested
fragments are either ‘presented’ or exocytosed

phagocytosis requires recognition of microbe via receptors for
PAMPs (pathogen associated molecular patterns - eg flagella or capsule) - recognised by toll-like receptors
activated complement
antibody
The innate immune response primes for the adaptive
B-cells are primed by activated complement
Th1 cell differentiation needs pro-inflammatory cytokines
Tick vectors
Ixodes:
Lyme disease: Borrelia burgdorferi
Babesiosis: Babesia microti
Granulocytic Erlichiosis: Erlichia phagocytophila

Dermacentor:
Tularemia: Francisella tularensis
Rocky Mountain Spotted Fever: Ricketsia rickettsii
Colorado Tick Fever: CTFVirus (Reovirus)

Amblyomma (lone star tick)
Monocytic Erlichiosis: Erlichia chaffeensis



Medically Important Fungi

ONE STEP AT A TIME: Free Printable
Hellooo! Yesterday I reached 15.000 followers (!!!!!!!!!!), which is so, so crazy. I would have never ever expected that when I first created this blog, so THANK YOU ALL SO MUCH <3 I love every single one of you.
To celebrate, I decided to make some printables yayyyy!! It’s a weekly planner that comes in the following options: blank, lined, graph and 2 columns (lined). Also I made portuguese versions yeahhh
Download links:
English: blank / lined / graph / 2 columns
Português: branco / pautado / quadriculado / 2 colunas
If you have any problem with it, please let me know. And also tag me if you use it! x

Immunosupressants Drug Mnemonic
Bc everything’s better when I study with Harry Potter references.
I’m reposting it, because I love this chart


20 09 18
i feel as though i haven’t been as active these past couple of days. uni and work just drained the life out of me and i haven’t done anything but lay in bed when getting home.
on the bright side, i did force myself to get up and clean my room. so here are some low-light pics of my bedroom :)
Antimicrobial Agents - Inhibition of DNA and Protein Synthesis
Bacterial chromosome replication

DNA replication

Bacterial Topoisomerases
maintain DNA in appropriate state of supercoiling
cut and reseal DNA
DNA gyrase (topoisomerase II) introduces negative supercoils
Topoisomerase IV decatenates circular chromosomes
these are the targets of the quinolone antibacterial agents
Quinolones
bind to bacterial DNA gyrase and topoisomerase IV after DNA strand breakage
prevent resealing of DNA
disrupt DNA replication and repair
bactericidal (kill bacteria)
Fluoroquinolone is particularly useful against
Gram +ves: Staphylococcus aureus, streptococci
Gram -ves: Enterobacteriacea; Pseudomonas aeruginosa
Anaerobes: e.g. Bacteroides fragilis
many applications e.g. UTIs, prostatitis, gastroenteritis, STIs
Adverse effects
Relatively well tolerated
GI upset in ~ 5% of patients
allergic reactions (rash, photosensitivity) in 1 - 2% of patients

Inhibition of Bacterial Protein Synthesis
Macrolides
in 1952: Erythromycin was isolated as the first macrolide (Streptomyces erythreus)
Newer macrolides: clarithromycin, azithromycin
Structurally they consist of a lactone ring (14- to 16-membered) + two attached deoxy sugars
Mode of action
bind reversibly to bacterial 50S ribosomal subunit
causes growing peptide chain to dissociate from ribosome → inhibiting protein synthesis
bacteriostatic (stops reproduction)

Macrolides’ spectrum of activity
good antistaphylococcal and antistreptococcal activity
treatment of respiratory & soft tissue infections and sensitive intracellular pathogens • e.g. Chlamydia, Legionella
Adverse effects
Generally well tolerated
nausea
vomiting
diarrhoea
rash
Aminoglycosides
large family of antibiotics produced by various species of Streptomyces (“mycin”) and Micromonospora (“micin”)
include: streptomycin, neomycin, kanamycin, gentamicins, tobramycin
Structure = linked ring system composed of aminosugars and an aminosubstituted cyclic polyalcohol
Mode of action of aminoglycosides
Bind irreversibly to 30S ribosomal subunit
disrupt elongation of nascent peptide chain
translational inaccuracy → defective proteins
bactericidal

Spectrum of activity
broad spectrum; mainly aerobic G-ve bacilli (e.g. P. aeruginosa)
used to treat serious nosocomial infections (hospital acquired infections)
First TB antibiotic
Used for cystic fibrosis
Adverse effects
all aminoglycosides have low Therapeutic Index (only a small amount needed to become toxic)
renal damage, ototoxicity, loss of balance, nausea



Medically Important Bacteria: Clasification
Elek test to document toxi production of Corynobacterium diphteriae
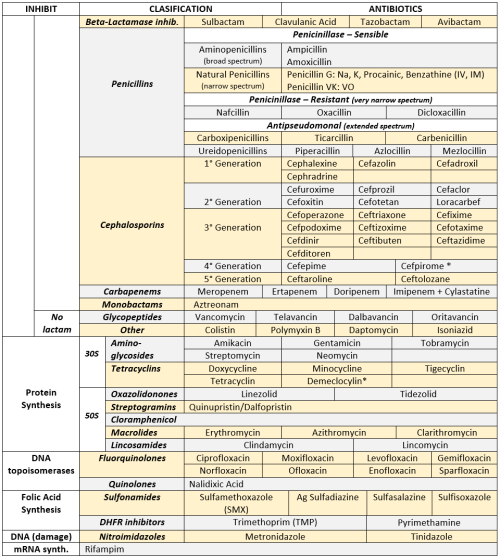
ANTIBIOTICS CHEAT SHEET :)
Also, REMEMBER!!!!
* Sulfonamides compete for albumin with:
Bilirrubin: given in 2°,3°T, high risk or indirect hyperBb and kernicterus in premies
Warfarin: increases toxicity: bleeding
* Beta-lactamase (penicinillase) Suceptible:
Natural Penicillins (G, V, F, K)
Aminopenicillins (Amoxicillin, Ampicillin)
Antipseudomonal Penicillins (Ticarcillin, Piperacillin)
* Beta-lactamase (penicinillase) Resistant:
Oxacillin, Nafcillin, Dicloxacillin
3°G, 4°G Cephalosporins
Carbapenems
Monobactams
Beta-lactamase inhibitors
* Penicillins enhanced with:
Clavulanic acid & Sulbactam (both are suicide inhibitors, they inhibit beta-lactamase)
Aminoglycosides (against enterococcus and psedomonas)
* Aminoglycosides enhanced with Aztreonam
* Penicillins: renal clearance EXCEPT Oxacillin & Nafcillin (bile)
* Cephalosporines: renal clearance EXCEPT Cefoperazone & Cefrtriaxone (bile)
* Both inhibited by Probenecid during tubular secretion.
* 2°G Cephalosporines: none cross BBB except Cefuroxime
* 3°G Cephalosporines: all cross BBB except Cefoperazone bc is highly highly lipid soluble, so is protein bound in plasma, therefore it doesn’t cross BBB.
* Cephalosporines are "LAME“ bc they do not cover this organisms
L isteria monocytogenes
A typicals (Mycoplasma, Chlamydia)
M RSA (except Ceftaroline, 5°G)
E nterococci

* Disulfiram-like effect: Cefotetan & Cefoperazone (mnemonic)
* Cefoperanzone: all the exceptions!!!
All 3°G cephalosporins cross the BBB except Cefoperazone.
All cephalosporins are renal cleared, except Cefoperazone.
Disulfiram-like effect
* Against Pseudomonas:
3°G Cef taz idime (taz taz taz taz)
4°G Cefepime, Cefpirome (not available in the USA)
Antipseudomonal penicillins
Aminoglycosides (synergy with beta-lactams)
Aztreonam (pseudomonal sepsis)
* Covers MRSA: Ceftaroline (rhymes w/ Caroline, Caroline the 5°G Ceph), Vancomycin, Daptomycin, Linezolid, Tigecycline.
* Covers VRSA: Linezolid, Dalfopristin/Quinupristin
* Aminoglycosides: decrease release of ACh in synapse and act as a Neuromuscular blocker, this is why it enhances effects of muscle relaxants.
* DEMECLOCYCLINE: tetracycline that’s not used as an AB, it is used as tx of SIADH to cause Nephrogenic Diabetes Insipidus (inhibits the V2 receptor in collecting ducts)
* Phototoxicity: Q ue S T ion?
Q uinolones
Sulfonamides
T etracyclines

* p450 inhibitors: Cloramphenicol, Macrolides (except Azithromycin), Sulfonamides
* Macrolides SE: Motilin stimulation, QT prolongation, reversible deafness, eosinophilia, cholestatic hepatitis
* Bactericidal: beta-lactams (penicillins, cephalosporins, monobactams, carbapenems), aminoglycosides, fluorquinolones, metronidazole.
* Baceriostatic: tetracyclins, streptogramins, chloramphenicol, lincosamides, oxazolidonones, macrolides, sulfonamides, DHFR inhibitors.
* Pseudomembranous colitis: Ampicillin, Amoxicillin, Clindamycin, Lincomycin.
* QT prolongation: macrolides, sometimes fluoroquinolones
-
 lujainblr reblogged this · 3 years ago
lujainblr reblogged this · 3 years ago -
 lakikuli liked this · 4 years ago
lakikuli liked this · 4 years ago -
 starsinplainsight liked this · 4 years ago
starsinplainsight liked this · 4 years ago -
 cosmodisasters liked this · 4 years ago
cosmodisasters liked this · 4 years ago -
 mipk90 liked this · 4 years ago
mipk90 liked this · 4 years ago -
 hobbithoard reblogged this · 5 years ago
hobbithoard reblogged this · 5 years ago -
 juicywizards liked this · 5 years ago
juicywizards liked this · 5 years ago -
 l-obird liked this · 5 years ago
l-obird liked this · 5 years ago -
 got-no-username liked this · 5 years ago
got-no-username liked this · 5 years ago -
 121gabby liked this · 5 years ago
121gabby liked this · 5 years ago -
 impulsiveliahthoughts reblogged this · 5 years ago
impulsiveliahthoughts reblogged this · 5 years ago -
 softcliche liked this · 5 years ago
softcliche liked this · 5 years ago -
 fallling-slowly liked this · 5 years ago
fallling-slowly liked this · 5 years ago -
 loveabounded liked this · 5 years ago
loveabounded liked this · 5 years ago -
 turcerp-blog liked this · 5 years ago
turcerp-blog liked this · 5 years ago -
 weaverboos liked this · 5 years ago
weaverboos liked this · 5 years ago -
 eyes-on-optom reblogged this · 5 years ago
eyes-on-optom reblogged this · 5 years ago -
 eyes-on-optom liked this · 5 years ago
eyes-on-optom liked this · 5 years ago -
 shinakazami1 liked this · 5 years ago
shinakazami1 liked this · 5 years ago -
 ets-2023-blog liked this · 6 years ago
ets-2023-blog liked this · 6 years ago -
 ourvisiontouchedthesky liked this · 6 years ago
ourvisiontouchedthesky liked this · 6 years ago -
 izzybooksit-blog liked this · 6 years ago
izzybooksit-blog liked this · 6 years ago -
 impromptuinterest liked this · 6 years ago
impromptuinterest liked this · 6 years ago -
 erin-spradlin-blog liked this · 6 years ago
erin-spradlin-blog liked this · 6 years ago -
 peter-granger reblogged this · 6 years ago
peter-granger reblogged this · 6 years ago -
 hwanggeumholang reblogged this · 6 years ago
hwanggeumholang reblogged this · 6 years ago -
 hwanggeumholang liked this · 6 years ago
hwanggeumholang liked this · 6 years ago -
 t-b-a-blr-blog reblogged this · 6 years ago
t-b-a-blr-blog reblogged this · 6 years ago -
 t-b-a-blr-blog liked this · 6 years ago
t-b-a-blr-blog liked this · 6 years ago -
 absolutelysuperb liked this · 6 years ago
absolutelysuperb liked this · 6 years ago -
 drunkinhigh liked this · 6 years ago
drunkinhigh liked this · 6 years ago -
 longlivepurplesloth liked this · 6 years ago
longlivepurplesloth liked this · 6 years ago -
 human------------being liked this · 6 years ago
human------------being liked this · 6 years ago -
 impulsiveliahthoughts liked this · 6 years ago
impulsiveliahthoughts liked this · 6 years ago -
 awkwardly-yours reblogged this · 6 years ago
awkwardly-yours reblogged this · 6 years ago -
 echoesofwinter liked this · 6 years ago
echoesofwinter liked this · 6 years ago -
 zuko-studies liked this · 6 years ago
zuko-studies liked this · 6 years ago -
 ode-to-phame liked this · 7 years ago
ode-to-phame liked this · 7 years ago -
 bluepineforests reblogged this · 7 years ago
bluepineforests reblogged this · 7 years ago -
 cancerousbib reblogged this · 7 years ago
cancerousbib reblogged this · 7 years ago -
 eyepedia-blog liked this · 7 years ago
eyepedia-blog liked this · 7 years ago -
 angelofnectar liked this · 7 years ago
angelofnectar liked this · 7 years ago